|
Recived: 20.01.2015
Accepted: 25.02.2015
Original
article
|
Abstract
|
|
|
|
International
Classification of Functioning, Disability, and Health (ICF, WHO, 2001) is a
constructive framework for quality assessment and treatment in Logopedics
(Speech Language Therapy). The current research study makes an attempt to
introduce this standard into logopedical practice and applied research to
measure the quality of life of persons with fluency disorders, such as
stuttering. The quality of life is a modern multidimensional construct that covers health-medical, psychological, social and economic
factors. Good level of communication and stabilized
fluency is of key
importance to improve the quality of life of persons who stutter.
The purpose of the study was
to show a model of assessment, treatment and evaluation of the efficacy of
the non-avoidance approach in adult stuttering therapy.
|
|
Methods: CharlesVan Riper’s non-avoidance approach for an
intensive therapy. Participants were 15 adults who stutter with an
average age 25.2 years.
Results: Specific
significant decreasing of the two main parameters: index of dysfluencies
immediately after the intensive therapy as well as duration of disfluences in
seconds. The changes in speech fluency before and after the intensive therapy
as well as 3 years after this therapy were obtained regarding the duration of
disfluencies and index of dysfluency.
Conclusion: The
present model of an intensive non-avoidance therapy format for adults with stuttering disorders was
successfully applied for the Bulgarian conditions. Improved fluency is an
important factor for quality of life improvement of persons with stuttering
disorder.
|
|
|
|
Keywords: International Classification of Functioning, Disability, and Health
(ICF); fluency disorders; stuttering; stuttering therapy; evidence-based practice;
quality of life; outcomes measures.
|
|
|
|
Introduction
|
|
|
|
Research status in the relevant topic in Bulgaria
According to WHO the understanding of the ICF model in respect to
stuttering as a type of fluency disorder requires interdisciplinary
interpretation and competence (1).
The application of the ICF is a constructive framework for quality
diagnostics and speech therapy of stuttering in many advanced countries in
the EU, the U.S. and Australia. It
is known that Yaruss and Quesal (2)
adapted the ICF for the needs of Logopedics (Speech-Language Pathology or
Therapy). They propose that the classification should be adopted as a framework
for reporting the speech therapy efficiency in relation to stuttering. The
ICF model describes how stuttering can be viewed according to the following
perspectives: (i) presumed
etiology, (ii) impairment in body function (observable stuttering behaviors),
(iii) personal factors and affective, behavior and cognitive reactions, (iv)
environmental factors, (v) activity limitations and participation restrictions.
Unfortunately, in Bulgaria
there are no research and science-based measurements of speech and language treatment services with the use of the ICF model. The National Scientific
Fund of Bulgaria (the
NSF) has funded only one highly successful research project in the professional
field of Public Health and Logopedics (2009-2012, contract number DTK 02/33).
It was about Evidence-Based Practice in Fluency and Voice Disorders, directed by D. Georgieva, South-West University “Neofit Rilski”. The
outcomes of intensive speech therapy with people of all ages who stutter were
published in peer reviewed international journals (3, 4, 5). Medical
treatment, health communication, social and psychological services for people
who stutter were applied to enhance the quality of life of clients from the
South-western region of Bulgaria, which include the capital, Sofia. A long
term goal of the study was to encourage the development of health tourism in the area, which is
defined as a region of health in a number of projects under the Sixth and
Seventh EU Framework Program.
The stuttering outcome is a
change in the client’s current and future fluency status that can be attributed
to antecedent health care (6). Outcomes refer to the effects of therapy,
programs or policies in individuals or population. Outcomes may also be
defined as changes in status attributed to a specific intervention or
therapy.
Within the proposed study
below, an attempt is made aiming to introduce this ICF standard practice in Logopedic and Logopedic applied research for measuring the multiple outcomes in individuals with stuttering.
|
|
|
|
Relevance of scientific problems in Bulgaria
and Europe
The EU Statistics Classification was accepted in Bulgaria in
2008. According to the EU Statistics Classification of 1999 and its
methodological handbook ISCED 97 Logopedics (Speech Language Therapy) is
considered a health profession and is located in professional direction 726
physiotherapy and rehabilitation. As a new member of the EU, Bulgaria
undoubtedly adheres to these rules. In July 2009, the Speech Language Therapy
program at South-West University in Blagoevgrad,
Bulgaria
successfully completed the official procedure of accreditation and evaluation
as part of the health sciences professions. This act created the required
conditions for conducting significant research in the field of Speech
Language Pathology following the ICF model.
Some
statistical data on communication, speech and language disorders in Bulgaria: 2.5% of the country’s total
population, or 150 000 people, are affected by stuttering or other
dysfluency type. 4% of school aged children suffer from stuttering (7). The
Bulgarian healthcare system offers no logopedic treatment for adolescents and
adults who stutter. In a number of international publications and world congresses,
the country is being criticized for not offering speech therapy service to
adult persons who stutter (8–11). The criticism, directed at the Bulgarian practice, enforced European
standards for the provision of quality speech therapy and development of
instruments for measuring the quality of life of persons with communication
disorders as a whole.
Bulgaria
participated successfully in a network project of 65 European universities,
funded by the European Social Fund entitled "Network for Tuning
Standards & Quality of Educational Program for Speech Language Therapists
in Europe" 2010–2013, Project number 177 075-LLp-1-2010-1-FR-EARSMUSENWA
(12) and was awarded a Fulbright research grant 2013 "Evidence-Based
Practice through Acoustic and Electroglottographic Characteristics Measuring
in Stuttering and Voice Disorders" - the only research project in the
field of speech therapy in Bulgaria won by the author of the present article
(13). In the frame of those projects the new paradigm “evidence-based
practice” in accordance with the ICF model was strongly recommended.
The new
concept for the application of the ICF classification in the field of
communication disorders (in the context of this current topic: stuttering) is
not known by Bulgarian speech language therapists. It is fundamental with
respect to speech language pathology science and therapy in some countries of
the European Union, the USA,
Australia and Canada. This
new paradigm refers to an approach in which the current, highly qualitative
research practiceс attempt to provide data not only about the clients' satisfaction
from the comprehensive speech service, but also about the clients' quality of
life. In Bulgaria,
in general, no systematic publications on the problem have been published,
even though in the European (CPLOL) and international (IALP) speech language
pathology organizations this model is specified as a standard.
The medical
model of stuttering seeks to reveal the causes and to provide proper therapy
for the persons with this communication disorder. Published scientific
studies in the U.S., Canada, Australia; England draw attention to the
diagnosis of the external, visible characteristics of stuttering and puts
minor emphasis on the evaluation of the experience of the person who stutters
as a speaker (14–17).
The social, psychological and logopedical model focuses on the inclusion of
the person who stutters in the society and also emphasizes the quality of
his/her life.
The review
of the Bulgarian literature indicated a lack of knowledge of the ICF model in
the country (see Table 1).
Table
1. Application of the International Classification of
Functioning, Disability, and Health - ICF, WHO, (1)
abroad and in Bulgaria,
comparative analyses regarding the stuttering disorder studies
|
|
ICF-компоненти /
The ICF components
|
САД, Австралија, Канада, Англија
/ The USA,
Australia, Canada, England
|
Бугарија /
Bulgaria
|
|
Нарушувања на телесната функција / Body function disorders
|
Conture (18); Johnson (19); Riley (20);Yairi and Ambrose (21)
|
Не / No
|
|
Нарушувања на телесната структура / Body structure disorders
|
Chang, Erickson,
Ambrose, Hasegawa-Johnson, & Ludlow
(22); Foundas, Bollich, Corey, Hurley, & Heilman (23)
|
Не / No
|
|
Индивидуално- контекстуални фактори / Individual
contextual factors
|
Cooper (24);
Manning (25); Shapiro (26); Sheehan (27); Van Riper (28); Watson (29)
|
Не / No
|
|
Контекстуални фактори на животната средина / Environment-based contextual
factors
|
Craig A, Hancock
K, Tran Y, & Craig M (30); Klein & Hood (31); Brutten & Shoemaker
(32); Ornstein & Manning (33); Woolf (34); Wright & Ayre (35); Ayre
& Wright (36) Yaruss
& Quesal (2); Yaruss (38)
|
Georgieva, (9), K. O. St. Louis, Filatova, Coskun,
Topbas, Ozdemir, Georgieva, McCaffrey,
George (37)
|
|
Ограничувања во активностите и рестрикции на
учество / Activity limitations and participation restrictions
|
Некои автори од САД и Австралија сметаат дека
квалитетот на животот е концепт поврзан со пелтечењето: Craig et al., (39);
Klompas & Ross (40) / Some authors from the USA and Australia consider
the quality of life as a concept, related to stuttering: Craig et al., (39);
Klompas & Ross (40).
|
K. O. St. Louis, Filatova, Coskun, Topbas, Ozdemir, Georgieva, McCaffrey,
George (41); Georgieva, Fibiger (3); Georgieva (4, 5).
|
Легенда: / Legend:
|
Медицински модел на
интерпретација на пелтечењето според МКФ / Medical model of stuttering interpretation according
to ICF
|
|
Логопедски и психолошки
модел на интерпретација на пелтечењето според МКФ / Logopedical and psychological model of stuttering
interpretation according to ICF
|
|
Логопедски и
социjален модел на интерпретациjа на пелтечењето според МКФ / Logopedical and
social model for stuttering interpretation according to ICF
|
|
This fact makes the scientists and
especially speech language therapists recognize the need for broad-based
implementation of evidence-based assessment and therapy for this complex
communication disorder.
The
purpose of the current study was to develop an ICF model of assessment,
therapy and evaluation of the efficacy of the applied treatment approach in
adult stuttering cases.
|
|
|
|
Present Study
Methodology
|
|
|
|
This research study was
built on the ICF model (1), which is a standard for speech therapists,
according to the IALP guidelines for initial education in Speech-Language
Pathology and the standards for practicing the clinical Logopedic profession
(42–44).
Methods
Charles Van Riper’s non-avoidance approach for an
intensive therapy (IT) format for
adults was applied (45). Full and detailed description of the study
procedures were published by Georgieva and Fibiger (3), Georgieva (4) and Georgieva (5).
|
|
|
|
Basic
considerations
The design of the therapy program was elaborated by Steen Fibiger and
was based on the following considerations:
ü Van Riper’s stuttering modification approach
was applied.
ü The team of speech therapists consider
motivation as a major element in the adult stuttering therapy (AST). A lack
of motivation was observed for one adult. The possible explanation was a
reflection of discouragement because of the ‘poor” results of the precedent
treatment.
ü WASSP Summary Profile was applied as a way of
measuring change in feelings, thoughts and behaviors and planning future management
(35, 36). This profile aims to record how the person who stutters perceives
his or her stuttering at the beginning and the end of a block of speech and
language therapy. WASSP
is an indicator for improvement in the quality of life after the therapy
period.
ü The AST requires involvement of four speech language therapists.
ü The official training language was Bulgarian, but all of the
participants were fluent in English.
Specific therapy methods for assessment (SSI-3)
and treatment of stuttering in adults, as well as measurement of the
effectiveness of Logopedic interventions (46) were also conducted.
The
application of voice acoustic analysis of the voice of adults who stutter has
also been planned using computerized speech laboratory (CSL) and specific
softwares as RTP (Real Time Pitch), and EGG
(electroglottography), (47, 48). To take these measures in voice disorders
is not obligatory but advisable.
It is intended
to use these various tools in the field of Public Health - Logopedics to
achieve fluent speech (for a detailed
description see Table 2 below).
|
|
Table 2. ICF components, providing a detailed stuttering description in the current research
|
|
|
|
Преглед на МКФ-компоненти во проектот / ICF components for project examination
|
Препорачани специфични дијагностички алатки за евалуација на
ефективноста од логопедската терапија според Yaruss, (49, 50) / Recommended specific
diagnostic tools for evaluating the effectiveness of the speech intervention on Yaruss, (49, 50)
|
|
Оценка и дијагностика на нарушувањето на флуентноста / Fluency disorder assessment and diagnosis
|
Инструмент за
евалуација на степенот на тежина на пелтечењето, чиј автор е Riley, (46) / Stuttering
Severity Instrument SSI-3,
authored by Riley, (46)
|
|
Оценка на реакциите на пелтечењето / Assessment
of stuttering reactions
|
1.
S-24
Andrews & Cutler (51
2.
Скала за пресметување на самоувереноста на
возрасни кои пелтечат при пристапување и одржување на флуентноста во различни
говорни ситуации (Ornstein
& Manning, 52) / Self-Efficacy
Scale for Adults Who Stutter (Ornstein & Manning, 52)
|
|
Истражување на
самооценката на лица кои пелтечат / Research on the stutterer's self-assessment
|
Профил за самооценка при пелтечење Write & Ayer (35, 36) /
Write & Ayer Stuttering Self Rating Profile
(
35,36)
Протоколи на Crove (53) / Crowe’s
Protocols (53)
|
|
Детална оценка на
говорното искуство на лицето кое пелтечи - мерење на квалитетот на животот / Comprehensive diagnosis of the speech experience of
the person who stutters - measuring the quality of life
|
Севкупна оценка на
искуството кое лицето го има од своето пелтечење - Yaruss and Quesal, (2, 54) – во процес на превод и адаптација за бугарски
услови / Overall
Assessment of the Speaker’s Experience of Stuttering -Yaruss and Quesal, (2, 54) – in process of translation and
adaptation for Bulgarian conditions
|
Specific research activities
The main goal of
the present study was to assess therapy outcomes using a variety of stuttering
measurements based on Van Riper’s intensive therapy
approach. Second research was conducted to specify any changes that are adopted in different
speech situations (in the stabilization phase), and to demonstrate that changes
are maintained after the therapy (1, 2, and 3 years after the treatment).
Measurement
for adults includes determination of index
of dysfluencies (ID) - the number of stuttering events divided by the
number of syllables, and duration of
dysfluences (DDs) - in seconds, for the three longest stuttering events.
Specific
stuttering measurements:
Application of SSI - 3 developed by Riley (46) – (Table
2 and
Table 3).
|
Table 3. Stuttering
Severity Instrument for Adults – results after the assessment before the
intensive treatment
|
|
|
|
|
Клиент / Client
|
Пол / Gender
|
Почетен SSI-резултат
(процент) / Initial
SSI score (percentage)
|
Почетен степен на тежина / Initial severity
|
|
S1
|
Ж / F
|
27 (60%)
|
Умерен / Moderate
|
|
S2
|
М / M
|
25 (41%)
|
Умерен / Moderate
|
|
S3
|
М / M
|
37 (96%)
|
Многу тежок /
Very severe
|
|
S4
|
М / M
|
46 (99%)
|
Многу тежок
/ Very
severe
|
|
S5
|
М / M
|
46 (99%)
|
Многу тежок
/ Very
severe
|
|
S6
|
Ж / F
|
27 (60%)
|
Умерен / Moderate
|
|
S7
|
М / M
|
25 (41%)
|
Умерен / Moderate
|
|
S8
|
М / M
|
46 (99%)
|
Многу тежок
/ Very
severe
|
|
S9
|
М / M
|
34 (88%)
|
Тежок / Severe
|
|
S10
|
М / M
|
35 (89%)
|
Тежок / Severe
|
|
S11
|
Ж / F
|
28 (61%)
|
Умерен / Moderate
|
|
S12
|
М / M
|
31 (77%)
|
Умерен / Moderate
|
|
S13
|
М / M
|
46 (99%)
|
Многу тежок
/ Very
severe
|
|
S14
|
М / M
|
35 (89%)
|
Тежок / Severe
|
|
S15
|
М / M
|
34 (88%)
|
Тежок / Severe
|
Легенда
/ Caption: Ж(женски); М (машки); SSI = степен на тежина за пелтечењето / F = female; M = male;
SSI = Stuttering severity instrument
|
Participants: Fifteen adults who stutter participated (average age
was 25.2 years). All of them had
experienced fluency shaping therapy prior to the current intensive stuttering
modification therapy (averaging 12.6 years prior to the present study; range
= 4–23 years). One participant had stuttering modification therapy (one year
prior to participation in the intensive course).
Inclusion criteria: To participate, adults who stutter had to (i) be older than 20
years; (ii) have taken part in a previous treatment trial, and (iii) have
exhibited a range of stuttering severities that ensured the sample was
representative.
Data collection: Each client’s files were
reviewed (assessment reports and
progress reports). Three types of files were recorded during the initial assessment,
at the onset of IT, and the end of the five day intensive therapy, 1, 2, and
3 years after the IT.
Measurements: (i) Changes in speech fluency the 1st, 2nd and 3rd year after the intensive treatment with adult stutterers. Evaluation
of stuttering severity was based on stuttering frequency during oral reading
and spontaneous speaking. The data collection mentioned above consists of two
fluency and affective-based measurements, which were assessed before
intensive treatment and immediately after the intensive treatment, as well as
1, 2, and 3 years after the IT.
Precision of measures refers to
the exactness with which stuttering dysfluencies can be measured.
|
|
|
Reliability of measures: After the IT and each of the
stabilization phase sessions, a five-minute video-recorded spontaneous speech
sample was obtained from each of the participants. Each speaking sample
contains at least 300-400 syllables to ensure reliable results. External independent
evaluation was provided by an independent clinician. He reported “measurement
agreement” 95%.
Validity: predictive validity
(criterion validity) is a gold standard because it refers to the ability to
predict future measures. At the end of the intensive adult stutterers'
therapy we could accurately predict whether clients would maintain their
gains.
Evidence-based practice: A good clinical practice should and must be
based on evidence. The clients’WASSP profiles were analysed individually.
The study offers a quantitative measure not necessarily requiring
normative comparisons regarding 2011
and 2012 – the so-called post treatment
period.
Statistics methods: The data obtained were
calculated using the Wilcoxon signed-ranks test for hypotheses testing.
|
|
|
|
|
|
Results and discussion
|
|
|
|
|
|
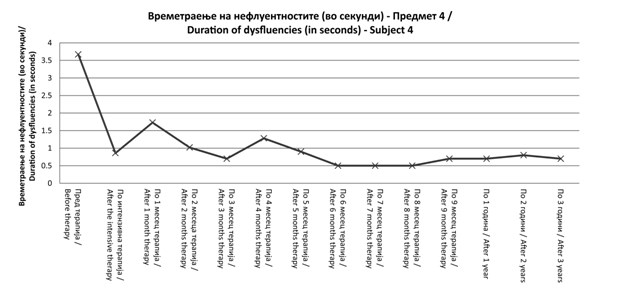
Changes in
speech fluency
Figure 1. Duration of
dysfluencies in seconds at the beginning versus end of the intensive treatment,
and one, two and three years after the intensive treatment for subject 4
|
At the beginning of the treatment
DD was 3.8 seconds and immediately
after IT this parameter reduced to 0.8 sec. Some changes in DD were observed over the first and second months
after the IT. For this client it was
difficult to maintain some of the new speech modification techniques like
pull-out and cancellation. The preparatory set technique was applied successfully
and stabilized by the client after 6 months of training after the IT. The
0.5sec DD increased slightly 3 years
after the IT.
Embarrassment, fears and anger
were typically presented after the student exam session. They characterized the so-called educational disadvantages of
client 4 and they are related to his poor educational achievements in that
period.
|
Figure 2. Duration of
dysfluencies in seconds at the beginning versus end of the intensive treatment,
and one, two and three years after the intensive treatment for all participants
(n=15), (5, 13)
The Wilcoxon signed ranks
test confirmed that there was a
reduction of DDs before and after intensive treatment (Z – 3.
408; p < 0.001):
§
Before IT and 1 year after IT (Z – 3. 408; p
< 0.001)
§
Before IT and
2 years after IT (Z – 3. 409; p < 0.001)
§
Before IT and
3 years after IT (Z – 3. 408; p < 0.001).
Sustained reduction in DDs was achieved (p < 0.001). There was
a significant reduction in the average duration of fluency disruptions.
There was a statistically significant
reduction of DDs:
§ After IT and 1 year after IT: (Z – 0.692; p < 0.489)
§ After IT and 2 years after IT: (Z – 0.684; p < 0.494)
After IT and 3 years after IT: (Z
– 1.329; p < 0.184).
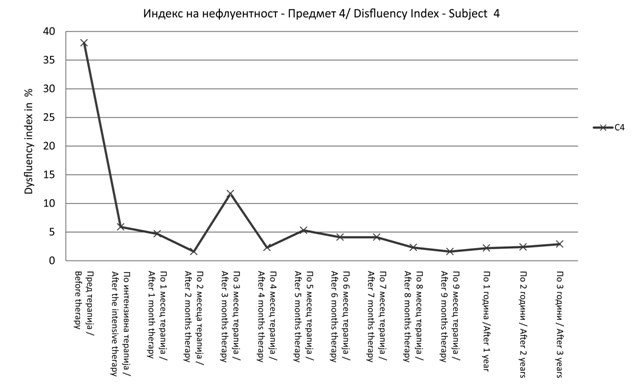
Figure 3. Dysfluency
index in % at the beginning versus end of the intensive treatment, and one,
two and three years after the intensive treatment for subject 4
Marked
decreases from 38% DI before
the IT to 6% after the treatment course. Two months after the IT in the stabilization phase the client manifested
low level of different types of disfluences with – only 0.3% variation in DI.
This means that he manifested fluent speech. There was a period of instability and variation of the DI curve where
the participant reverted to dysfluent speech (movements between 0.3% and a rapid increasing to 11.5%). From the client's files it was possible to show that he reported strong frustration
between the 2nd and 4th months after the IT, related to associated health problems. Subsequently,
the curve demonstrated strong maintenance of the fluent speech behavior and
stabilization of fluency 3 years after the IT. To summarize, the client needed a prolonged period of time to consolidate the
newly established speech behavior when the totally new speech techniques were
applied in this sensitive period. The overall pattern showed that in order to
stabilize the new stuttering behaviors acquired during the IT, continued
treatment and psychological and social support for a long period are needed.
Such long term support allows stabilization to continue and helps manage
relapses to the old stuttering behaviors.
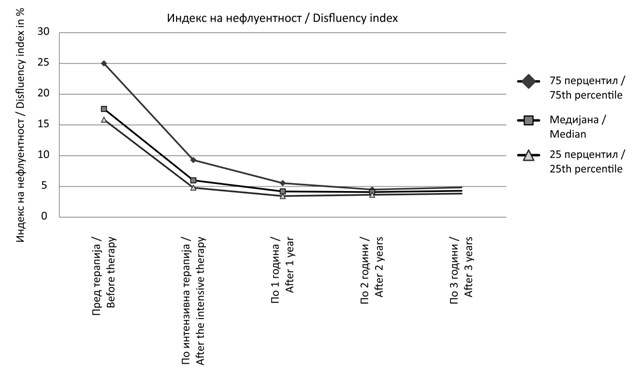
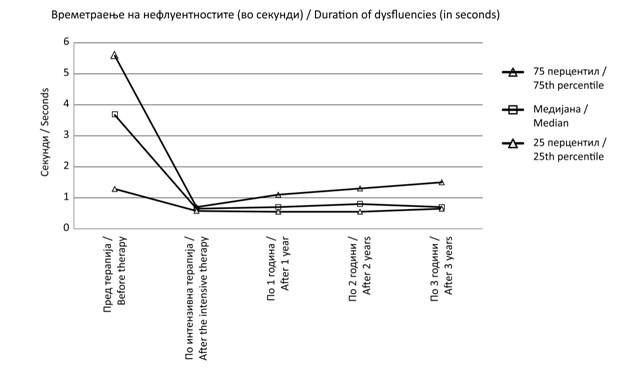
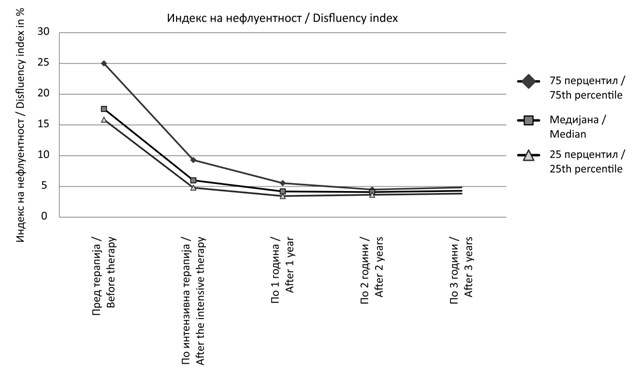
Figure 4. Dysfluency Index at the beginning versus end of the intensive therapy and one, two and three years after the intensive therapy for all
participants (n=15), (5, 13)
|
Significant changes regarding reduction of disfluency index were found
before and after intensive therapy (Z – 3.408; p < 0.001). DI before and after the IT show the next results:
§
Before
and after the 1st year (Z – 3.411; p < 0.001)
§
Before and after the
2nd year (Z – 3.408; p < 0.001)
§
Before
and after the 3rd year month (Z – 3.408; р < 0.001).
DI after the IT and
after 1, 2, 3 years post therapy show:
§ After
IT and after the 1st year (Z – 3.068; p < 0.002)
§
After IT and after
the 2nd year (Z – 3.408; p < 0.001)
§ After IT and after the 3rd year
month (Z – 3.202; р < 0.001).
|
|
|
|
WASSP Individual case results
Subject 4’s individual results and their
discussions are presented in this section. The initial SSI – 3 score was 46 (99%) which reflects very severe stuttering. The WASSP profile is shown in Figure 5.
The
WASSP profiles strongly support the observation of changes in the individual
stuttering behaviors before and after the IT as well as affective, emotional,
cognitive and social changes. In the individual case of client 4 (with very
severe initial stuttering) remarkable speech dysfluency changes were observed
immediately after the IT concerning all eight of the parameters examined.
Only one of the examinees’ WASSP profile parameters did not change after the
intensive course (negative thoughts during
speaking). This could be explained by the client’s inability to admit how
severe his stuttering was, as well as feelings and avoidance at the beginning
of the course. The changes were also impressive concerning Avoidance. The
present Van Riper’s non-avoidance approach requires
changes in the typical avoidance behavior through desensitization in
different speech situations. For the experienced clinician it is easy to observe decrease
of the avoidance attitude in all 4 areas: of words (from 6 to 3); of
situations (from 4 to 1); talking about stuttering with others (from 5 to 1),
and admitting problems to yourself (from 7 to 1). To conclude, client 4
reported a change of progress and reduction of scores for all five subscales
in WASSP.
|
WASSP-рејтинг
/ WASSP rating
sheet
|
|
Никој
/ None
|
Мн. тешко
/
Very
severе
|
|
|
1
|
2
|
3
|
4
|
5
|
6
|
7
|
|
Однесувања
при пелтечење /
Stuttering behaviors
|
Фреквенција на пелтечење /
Frequency of stutters
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Физичко водење борба при пелтечење / Physical struggle
during stutters
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Траење на пелтечењата /
Duration of stutters
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Неконтролирано пелтечење / Uncontrollable stutters
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Итност/стапка на брз говор /
Urgency/fast speech
rate
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Поврзани фацијални/телесни движења / Associated facial/body
movements
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Општо ниво на физичка тензија /
General level of
physical tension
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Губење на контактот со очи /
Loss of eye contact
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Друго / Other
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Мисли
/ Thoughts
|
Негативни мисли пред зборување / Negative thoughts
before speaking
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Негативни мисли во текот на зборувањето / Negative
thoughts during speaking
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Негативни мисли по зборувањето / Negative thoughts
after speaking
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Чувства
/ Feelings
|
Фрустрација / Frustration
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Срам / Embarrassment
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Страв / Fear
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Лутина / Anger
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Беспомошност / Helplessness
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Друго / Other
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Избегнување
/ Avoidance
|
Брз зборови / Of words
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Вон ситуација / Of situations
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Не се зборува со други за пелтечењето /
Of talking about
stuttering with others
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Непризнавање на проблемот на себеси /
Of admitting your
problem to yourself
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Недостаток
/ Disadvantage
|
Дома / At home
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Друштевн / Socially
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Едукациски / Educationally
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
На работа / At work
|
1
2
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
Забелешка: во третата колона: 1 - првата WASSP-евалуација; 2 = втората WASSP-евалуација (по интензивниот третман) /
Note:
in the 3rd column: 1= the first WASSP evaluation; 2=second WASSP
evaluation (after the intensive treatment)
|
Figure 5. Wright
& Ayer Stuttering Self-rating Profile (WASSP) summary of the client 4
|
|
|
|
His
explanatory comments in the last section of his profile revealed that he
had developed realistic expectations about stuttering outcomes. For
client 4, the fluency shaping approach had little or no lasting effect
which contrasted with the results of the non-avoidance approach in the
present study. The non-avoidance stuttering modification approach is
primarily a phenolmenological treatment, which is difficult to evaluate
in quantitative terms.
|
|
|
|
WASSP Group results
The set of WASSP subscales
results revealed considerable positive changes in response to participation
in the therapy course for the
majority of the participants. It includes behaviors, thoughts, feelings,
avoidance and disadvantage scales. They reported a visible change of
progress in all five subscales of the WASSP. The majority of clients were strongly motivated and reduced their degree of
stuttering from the
beginning of the intensive therapy. The rest of the WASSP
parameters changed in positive way.
|
|
|
|
Conclusion
|
|
|
|
The positive changes in speech
fluency before and after the intensive therapy and in the follow up period
(one, two and three years after the intensive therapy) were obtained
regarding the two essential parameters: (i) duration of dysfluencies, and
(ii) index of dysfluency (5, 13).
Improvement in stuttering
duration was observed immediately upon completing the intensive therapy. This
was reflected in a statistically significant reduction in the number of
stuttered utterances per minute. In the period of nine months stabilization
phase, one year, two years and three years after the therapy these positive
changes were maintained.
Although therapy was for a
limited time, this stuttering non-avoidance
approach intensive therapy provided the clients with new key experiences and
feelings that allowed them to progress based on their own effort.
Usually,
Bulgarian speech therapists prefer to apply fluency shaping approach and are
much more familiar with it. While the non-avoidance approach is a classic example of stuttering
modification approach to stuttering therapy, it is only one variant of many
stuttering modification therapies. We do not know whether these results can be
generalized to other stuttering modification approaches. Perhaps
simply participating in the present type of group stuttering intervention may
be sufficient to bring about the positive changes of the type and magnitude
that we observed
(5, 13).
Results from this study
showed that International Classification of Functioning, Disability, and Health
are a beneficial framework for quality assessment and therapy in logopedics regarding stuttering. This study introduced for the first time in Bulgarian logopedical
practice stuttering modification approach and represents a good example of
therapy outcomes evidence-based measurement.
|
Acknowledgement
This study was funded in the frame of the South-West
University “N. Rilski”, Blagoevgrad, Bulgaria research project: Evidence-based
stuttering management and measurement: Outcomes for a Camperdown stuttering
treatment (2015).
Conflict of
interests
Author
declare that have no conflict of interests.
|
References
|
|
|
|
|
|
|
|
1. International Classification of
Functioning, Disability, & Health. Geneva:
World Health Organization. 2001.
2. Yaruss JS, Quesal RW. Overall Assessment of the Speaker’s
Experience of Stuttering (OASES): documenting multiple outcomes in stuttering
treatment. J Fluency Disord 2006; 31: 90-115.
3. Georgieva D, Fibiger S. Intensive Non-avoidance Group Therapy with Adults
Stuterers: Experience from Bulgaria.
Dansk Audiologopaedi (Denmark).
2010 Sept; 3: 24–30.
|
|
4. Georgieva
D. Intensive Non-Avoidance Group Therapy with Adults Stutterers: Preliminary
Results. Proceeding of the International Conference of Stuttering (Editor Giacomo Soncini), Prima
edizione, 7-9 June, Roma: Omega Edizioni; 2012; 163–171.
5. Georgieva D. Intensive
Non-Avoidance Group Therapy with Adults Stutterers: Follow up Data. Proceedings
from the 10th Oxford Dysfluency Conference, St. Catherine college,
Oxford, UK; 2015, July (in press).
6. Golper LA, Frattali CM.
Outcomes in Speech Language Pathology. Second edition. NY: Thieme, 2013.
|
|
7. Ivanov
V. Logopedics. Sofia:
Nauka i izkustvo, 1973 (in Bulgarian).
8. Georgieva
D, Goranova E. The treatment of fluency disorders: experience in Bulgaria. Presentation
at the 7th Oxford
Dysfluency Conference; 2005.
9. Georgieva
D. Speech situations, increasing the degree of
stuttering in persons aged 13–16 – PhD thesis, Sofia University, Bulgaria; 1996.
10. Fibiger
S, Peters H, Euler H, Neumann K. Health and human services for persons who
stutter and education of logopedists in East-European countries. J Fluency
Disord 2008; 33: 66–71.
11. Fibiger S, Peters H,
Touzet, BB, Neumann K. Therapy for persons who stutter: Eastern Europe and Latin America. In: 5th World Congress on
Fluency Disorders, 25-28th July; 2006, Dublin, Ireland.
12. NetQues Project. Network for Tuning Standards & Quality of Educational Program for
Speech Language Therapists in Europe
funded by
ERASMUSENWA Life Long Learning Programme [online]
2010-2013 [cited 2014]. Available from: http://www.Netques.eu/?page
_id=44
13. Georgieva D. Non-avoidance Group Therapy
with Adults Stutterers: Preliminary Results. CoDAS, J of Sociedade
Brasiliera de Fonoaudiologia; 2014; 26 (2): 112–120.
14. Andrews
G, Guitar B, & Howie P. Meta-analysis
of stuttering treatment. J Speech Hear Disord 1980;45: 287–307.
15. Cordes
AK, Ingham RJ. editors. Treatment efficacy for stuttering: a search for
empirical bases. San Diego:
Singular Publ. Group; 1998, 213–242.
16. Prins D, & Ingham R. Evidence-based treatment
and stuttering – historical perspective. J
Speech Lang & Hear Res
2009; 52: 254–263.
17. Thomas C, & Howell P. Assessing efficacy of
stuttering treatment. J Fluency Disord 2001;
26: 311–333.
18. Conture EG. Stuttering: Its nature, diagnosis,
and treatment. Needham Heights,
MA: Allyn and Bacon. 2001.
19. Johnson W. Stuttering and what you can do
about it. Danville, IL:
Interstate; 1961.
20. Riley GD. Stuttering
severity instrument (4th edition). Austin, Texas:
PRO-ED; 2009.
21. Yairi E & Ambrose N. A longitudinal
study of stuttering in children: A preliminary report. J Speech Hear Res
1992; 35: 755–760.
22. Chang SE, Erickson KI, Ambrose NG, Hasegawa-Johnson MA & Ludlow
CI. Brain anatomy differences in childhood stuttering. NeuroImage 2008; 39:
1333–1344.
|
|
23. Foundas
AL, Bollich
AM, Corey DM, Hurley, M, & Heilman, KM. Anomalous anatomy of
speech-language areas in adults with persistent developmental stuttering.
Neurology 2001; 57: 207–215.
24. Cooper
EB. Chronic perseverative stuttering syndrome: A
harmful or helpful construct? Am J Speech Lang Path 1993; 2(3):11–15.
25. Manning WH. Clinical decision making in fluency disorders
(3rd ed). Clifton Park,
New York: Delmar/Cengage
Learning. 2010.
26. Shapiro DA. Stuttering Intervention. A Collaborative
Journey to Fluency Freedom (2nd ed). Austin, Texas:
Pro-ed; 2011.
27. Sheehan
JG. Stuttering: Research and therapy. New York: Harper and
Row; 1970.
28. Van
Riper C. The nature of stuttering (2nd ed). Englewood Cliffs, New
Jersey: Prentice Hall; 1982.
29. Watson JB. Exploring the attitudes of adults who stutter,
J Com Disord 1995; 28: 143–164.
30. Craig A, Hancock K, Tran Y, & Craig M. Anxiety levels in people who stutter: A
randomized population study. J Speech Lang Hear Res 2003; 46: 1197–1206.
31. Klein JF & Hood SB. The impact of
stuttering on employment opportunities and job performance. J Fluency Disord 2004; 29(4): 255–273.
32. Brutten GJ & Shoemaker DJ. A two-factor
learning theory of stuttering. In Travis LE (Ed), Handbook of speech pathology
and audiology. Englewood
Cliffs, NJ: Prentice Hall; 1971: 1035–1072.
33. Ornstein A & Manning W. Self-efficacy
scaling by adult stutterers. J Com Disor 1985; 18: 313–320.
34. Woolf G. The assessment of stuttering as
struggle, avoidance and expectancy. British J Disord Com 1967; 2: 158–171.
35. Wright
L, Ayre A. WASSP: Wright and Ayre Stuttering Self-rating Profile. Bicester:
Speechmark; 2000.
36. Ayre A, Wright L. WASSP: an international
review of its clinical application. Intern J
Speech Lang Path 2009;11(1): 83–90.
37. St Louis KO, Filatova Y, Coskun M, Topbas S, Ozdemir S, Georgieva D, McCaffrey E, George R. Public Attitudes Toward Cluttering and Stuttering
in Four Countries. Chapter in book “Psychology of Stereotypes”, Nova Science Publishers, Inc, New
York, 2011; 81-115.
38. Yaruss JS. Assessing
quality of life in stuttering treatment outcomes research. J
Fluency Disord 2010; 35: 190–202.
|
|
39. Craig A, Blumgart E, &
Tran Y. The impact of stuttering on the quality of life in adults who
stutter. J Fluency Disord 2009; 34 (2): 61–71.
40. Klompas M & Ross E. Life experience
of people who stutter, and the perceived impact of stuttering on quality of
life: Personal accounts of South African individuals. J Fluency Disord 2004;
29(4): 275–305.
41. St. Louis KO, Filatova Y, Coskun M, Topbas S, Ozdemir S, Georgieva D, McCaffrey E, George R.
Identification of cluttering and stuttering by the public in four countries.
Intern J Speech-Language Pathology;
2010;12 (6): 508–519.
42. IALP International Association of Logopedics and
Phoniatrics. Guidelines for initial education in logopedics (speech/language
pathology/ therapy, orthophony, etc.): Folia Phoniat Logop 1995; 47: 296–301.
43. IALP (2010) Education Guidelines (September 1, 2009): Revised
Guidelines for Initial Education in Speech-Language Pathology. Folia Phoniat Logop; 2010;62:210–216.
45. Van Riper C. The treatment of
stuttering. New Jersey: Prentice-Hall; 1973.
46. Riley
G. Stuttering severity instrument for children and adults. 3rd
edition. Austin:
Pro-Ed; 1994.
|
|
47. Georgieva D. Acoustic and Electroglottographic Voice
Characteristics in Stuttering: Data From Two Cases. Proceedings of the 10th
International Conference on Advances in Quantitative
Laryngology, Voice and Speech Research, June 3-4, Cincinnati, Ohio, USA. 2013a; 83–84.
48. Georgieva D. Acoustic and Electroglottographic Voice Characteristics in
Stuttering: Group Study. Proceedings of the 10th International Conference on Advances in Quantitative
Laryngology, Voice and Speech Research, June 3-4, Cincinnati, Ohio, USA; 2013b;
85–86.
49. Yaruss JS. Measuring multiple outcomes in
stuttering treatment. In: 7th
Oxford Dysfluency Conference, Oxford, 2005; 5–11.
50. Yaruss JS. Describing the consequences of
disorders: Stuttering and the International Classification of Impairment,
Disability, and Handicaps. J Speech Lang Hear Res 1998; 49, 249–257.
51. Andrews G, Cutler J. Stuttering
therapy: The relation between changes in symptom level and attitudes. J
Speech Hearing Disord; 1974, 34: 312–319.
52. Ornstein
A, Manning, W. Self-efficacy scaling by adult stutterers. J Com Disord
1985;18, 313–320.
53. Crowe
TA, Cooper EB. Clinician attitudes toward and knowledge of stuttering. J Com
Disord 1977;10: 343–357.
54. Yaruss JS, Quesal RW. Stuttering and the International
Classification of Impairment, Disability, and Health (ICF): An update. J Com
Disord 2004; 37: 35–52.
|
|
|
|
No comments:
Post a Comment